
Undeniably, dentists who can provide informed pain management are highly sought after. Because pain is complex and specific to each person, there is no easy solution. Your goal is to create a sustainable and pleasant relationship with your patient through optimal care. We’ll see that many prejudices can hinder effective treatment, however some new approaches can support you in your daily practice. Today, pain management is not only drug-based, it strongly involves the way you communicate.

Pain is a question of perception
Pain is a phenomenon produced by the brain, and there are as many ways to express pain as there are different people. Many factors contribute to pain’s variability: genetic inequality, gender, education, social background, culture, etc.
Since pain expression varies so much and depends on all of these components, empathy becomes trickier: people tend to only recognise pain they can identify with personally. Practitioners need to overcome certain prejudices in order to avoid leaving a part of their patient base on the sidelines. Pain experienced by women in particular is systematically underestimated and consequently, under-treated. When suffering from an identical medical case, women receive less morphine compared to men. Gender bias or misconceptions in relation to biological differences are a common occurrence inside the medical system, and have led doctors to believe that women exaggerate their pain reports. These differences have been highlighted in a number of studies.1
What’s more, a recent study has now confirmed that women are actually more sensitive to certain types of pain. For instance, they have twice the number of receptors in their face: women have 34, compared to 17 for men. This difference may support the claim that women exhibit a different sensitivity to pain. 2
Pain levels are also often underestimated for black patients and other ethnic minorities, notably due to misconceptions about biological differences, leading to a gap in treatment and patient care.
For example, one retrospective study found that black patients were significantly less likely than white patients to receive analgesics for extremity fractures in the emergency department (57% versus 74%), despite similar self-reported pain.3
Individuals may also express pain differently due to their cultural background. For instance, stereotypes on masculinity may prevent some men from expressing their pain effectively.4 Consequently, as a dentist, it’s crucial to remain attentive while delivering the highest degree of care. However, it is not always easy to know what to recommend in each situation. Recent studies have introduced new avenues for pain management in patient care.
New pain treatments
To ensure that your patients receive optimal pain management in your practice, there is now a whole range of new techniques for you to discover or explore in greater detail. Your patients are the only ones who can tell you what they are feeling. Their participation is crucial in assessing the intensity of the pain and the effectiveness of the proposed treatments. Accordingly, new ways of managing pain take the patient into account as a whole, by calling on all their physical but also mental resources. Good communication is now the key to optimizing the therapeutic relationship. In order to succeed in this challenge, here are some guidelines that will put you on the right path.
Use active listening to relieve pain
This technique covers two aspects:
Empathy
It is absolutely necessary to believe what your patient tells you about their pain. There is nothing imaginary in their perception, even if it seems exaggerated to you, it is their own experience of the pain, which may be amplified by emotion.
Knowledge sharing
As a dentist, it is best to establish a partner relationship with the patient. When you share your knowledge with them and explain procedures in detail, you involve them in their care and reassure them. So, before initiating a treatment procedure, explain its purpose, the different stages and subsequent treatment plan to your patient. Finally, invite them to ask you questions which you will respond to in a simple and precise manner. By gaining their overall trust, you can co-create an authentic and viable care plan that lowers patient anxiety so it has less of an impact on pain expression.
Using scales to express pain
You may use some tools to help a patient express their feelings of pain. Among the most frequently used 3, 4
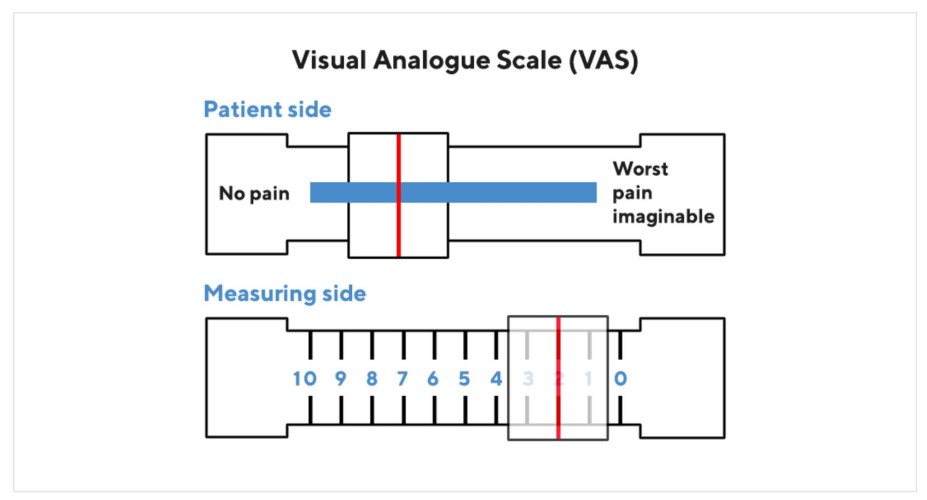
The Visual analogue scale (VAS)
A small ruler on which patients are asked to indicate their pain intensity by moving a cursor from one end to the other. The back of the ruler, designed for the assessor, has a scale from 0 to 10 (or 0 to 100 mm). However, just because two patients rate their pain between 7 and 10 does not mean that they will experience the same intensity. This assessment must be accompanied by a dialogue between the carer and patient.

The numeric rating scale (NRS)
The healthcare provider asks the patient to self-assess the current level of pain by circling the number from 0 to 10 that best describes their level of pain. A score of 0 is "no pain." A score of 10 is the "worst pain imaginable."
Both methods can be used to assess pain but can also be used to express a level of anxiety.
Soothing behavior and language
Learn to calm the patient's anxiety by being mindful of your choice of words. Healthcare received during childhood, or a bad experience can lead to unfounded fear. Your language, both verbal and non-verbal, will reassure the patient by being consistent. If you say, "I'm listening" your attitude should confirm this: don’t look out of the window or consult another file at the same time. This becomes obvious when you consider the "3V rule," based on studies published in 1967 by Professor Albert Mehrabian, according to which only 7% of communication is verbal (spoken word), 38% of this communication is vocal (tone and sound of voice), 55% is visual (facial expression and body language). This means that 93% of communication is non-verbal.5
However, words do have real power, especially when used in medical hypnosis. This is an increasingly popular technique in dental surgeries. This technique allows you to induce a state of relaxation in the patient, by fixing their attention elsewhere using a calibrated rhythm in your speech.
How to step out of your role
During your training, you may have learned to maintain a clinical distance and an even temperament. You may also have been advised not to get too close to your patients, for fear of absorbing their suffering and taking it on yourself. However, you have everything to gain by listening to your patients and exploring their needs by asking them questions.
Cognitive behavioural therapy (CBT)
When the pain has no discernible physical cause, how do you proceed as a practitioner? It might be of interest to explore its origin by using psychological therapies such as cognitive behavioural therapy. On the one hand, CBT focuses on relieving the manifestations of a psychological problem in order to get past the acute episode. On the other hand, it enables an in-depth study of patterns in the person's life. This in-depth work will not only lead to the understanding of the problems and their roots, but also to the modification of the dysfunctional patterns.
CBT is worth exploring both for patient comfort and practice productivity. This is because dental phobia can lead to repeated cancellations, constant rescheduling of appointments, or the inability to treat or reassure a very anxious patient. It may be a good idea for your practice to inform some patients about this type of behavioural therapy. Conducted by a psychologist, it is generally short and effective because it is tailored to a specific objective.
The integrative approach
When medication alone no longer helps patients, the aim is to help them become more autonomous in understanding and managing their pain. Integrative medicine combines standard treatments with alternative therapies such as acupuncture, mindfulness, massage or Qigong practice 7 . The first step is to educate and raise awareness of these techniques. Training courses are available for those who want to go further and integrate them into their practice.
Article Published in Dental Solutions Feb-March 2024
References
1 https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC3690315/
2 https://www.vidal.fr/maladies/douleurs-fievres/prise-chargedouleur/femme.html https://journals.lww.com/plasreconsurg/ Abstract/2005/ 10000/ Increased_Cutaneous_Nerve_Fibers_in_Female.31.aspx
3 https:/www.ncbi.nlm.nih.gov/pmc/articles/PMC4843483/
4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6157457
5 http://www.kaaj.com/psych/smorder.html
6 https://www.cairn.info/revue-hegel-2015-4-page-346.htm
7 Qigong, traditional Chinese gymnastics that combines slow movements, breathing exercises and concentration in the control of vital energy